It’s daunting and discouraging to feel lousy all the time. You know people who were diagnosed with COVID-19 and are already back to life at full speed. Why did they get better, but you didn’t?
Learning you’re infected with COVID-19 can be frightening. So, you did everything asked of you — you were even fortunate enough not to be hospitalized. Yet after you thought you’d recovered, some symptoms lingered. They puzzled you and your doctor. And, it turns out, you aren’t the only one who can’t quite kick COVID.

What is long-COVID?
Long-COVID — also known as, long-hauler COVID, post-COVID-19 inflammation syndrome, and from the CDC, post-acute sequelae of COVID-19 — is a set of symptoms or conditions that occur together after infection with the COVID-19 virus. There are multiple, potential symptoms and conditions that manifest physically, cognitively and emotionally.
Whatever you call it, post-COVID syndrome is a broad diagnosis for many symptoms that affect a lot of people. Shockingly, a recent health review concluded that over 50% of people who’ve had COVID-19 have related health issues for months after recovery. That’s a lot of long-COVID.
Symptoms of post-COVID conditions
Common prolonged aftereffects of COVID-19 infection include
- Brain fog
- Nagging cough
- Unrelenting fatigue
- Muscle and joint aches
- Shortness of breath
- Intestinal upset
. . . and more.
These persistent symptoms are clustered and referred to by many different names, including “long-COVID,” “long-haul COVID,” “chronic COVID,” “post-COVID syndrome,” “post COVID-19 condition” and “post-acute COVID-19 syndrome.”
Why do I still feel awful after COVID?
Before moving on, it’s important for you to know that the ViveWell medical team is here for you. We’re investigating the root causes of this new inflammatory syndrome by reading emerging research and comparing it with existing medical conditions and syndromes. We’re constantly learning about treatments that may decrease the waves of symptoms you and others endure.

The latest science on post-COVID conditions
Medical, health and other scientists are still learning about long-COVID’s causes. What we do know is that it impacts the body’s metabolism, inflammation and immunity. In fact, it affects almost every body system.
Oxidative stress, inflammation and COVID
The current scientific understanding of post-acute sequelae of COVID indicates it’s closely tied to a phenomenon known as oxidative stress in the metabolic system of each cell. Metabolism is how your body uses energy from the food you eat by processing the starches, fats, proteins, medications, drugs, alcohol, chemicals and environmental toxins.
During this cascade of metabolic chemical reactions, sometimes impurities in the body cause the formation of reactive substances. If your body is unable to handle them properly, these free radicals, or reactive oxygen species (ROS), trigger oxidative stress. You’ve likely read about antioxidants in foods or supplements that help to neutralize free radicals (or ROS) that harm cells.
Oxidative stress has many causes and accumulates as your body tries to compensate. Many people, unsurprised to learn that oxidative stress and inflammation combine to fuel painful diseases like arthritis, are unsettled to learn that this damaging duo also drives repeat infections and increases the risk of diabetes, heart disease, cancer and other conditions.
Even when healthy, your body continuously processes ROS from many sources. But when we fall ill, the balance tips. Oxidative stress is a result of:
- The environment
- A lack of nutrition in foods
- Various behaviors, like smoking
- Stress from everyday life — work, commuting, finances, lack of sleep, etc.
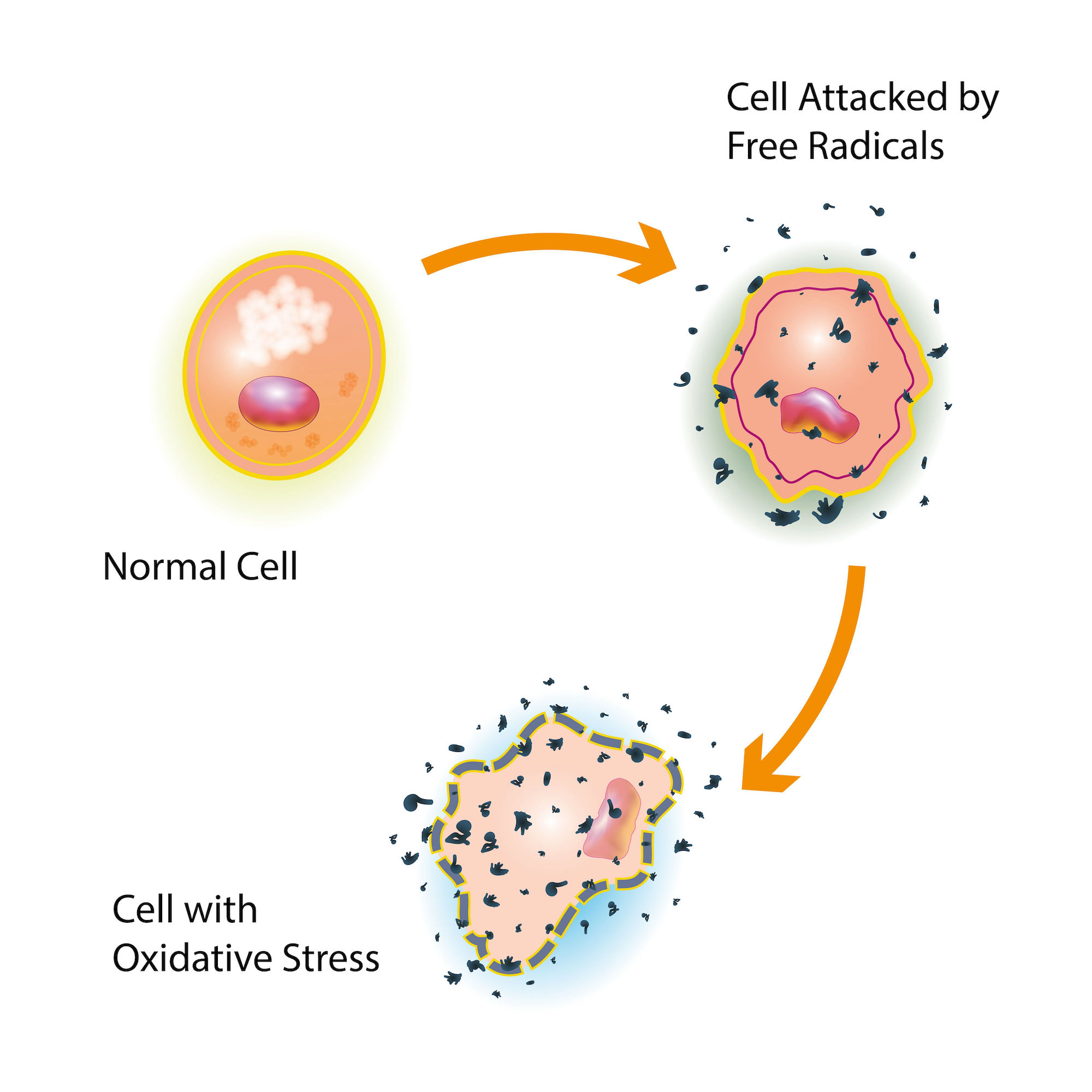
Oxidative reactions at the cellular level are closely tied to inflammation and its related chemical messages, cytokines. Medical scientists study the levels of different cytokines to discern how a virus like SARS-CoV-2 is affecting a person with the infection and long afterwards. There are different types of immune messages or cytokines. Some suppress parts of the immune system’s inflammatory processes, while others increase them.
A basic understanding of oxidative stress and inflammation is important when learning about the new science behind how COVID exposure can make someone feel unwell long after the acute infection has passed.
COVID and the immune response

As scientists work to better understand the COVID virus, there are a few important breakthroughs regarding how the virus affects the body and its immune response. Significantly, research has explored:
- The COVID spike protein and immune response
- Persistence of viral genetic material after infection
- Immune dysregulation
- Changes to the gut microbiome
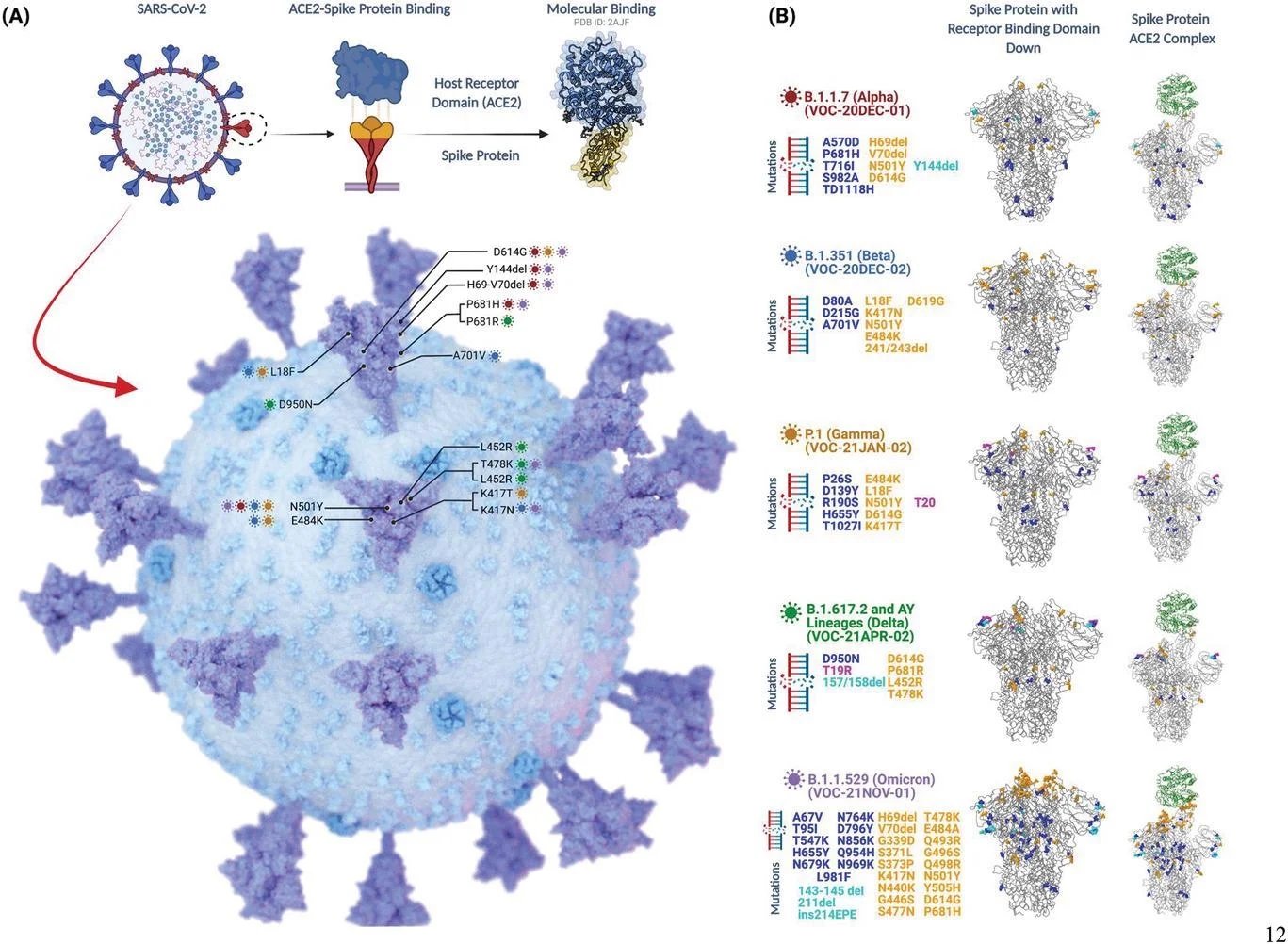
Scientific understanding of the COVID spike protein
The SARS-CoV-2 (COVID-19) spike protein, either from an infection or vaccination, can circulate throughout the body and its tissues, even crossing into the brain. Studies show the spike protein causes an immune response, triggering an inflammatory reaction that cascades through the body, disrupting the metabolic function of cells and causing inflammation within the endothelial cells that line blood vessels in every organ.
This immune response is responsible for blood clotting and implicated in the increase in cardiovascular disease, stroke, diabetes, persistant lung damage and brain damage. Because spike proteins trigger inflammation throughout the body, this may explain why people document over 200 different symptoms of COVID-19.
The complexities of a mutating virus
Part of your body’s immune response is to create antibodies that match the specific genetic sequence of the COVID-19 spike protein you were exposed to, either from infection or vaccination. This is similar to a “lock and key” model. The continuous genetic mutation of SARS-Cov-2 virus from the original “alpha” variant has occurred mostly in the spike protein. Evolving genetic sequence changes in the “variant of concern” spike protein. The “keys” on the spike protein no longer “unlock” the antibody immune response as well as in the past because of an antigen mismatch.
Successive spike protein mutations of each variant have caused differing immune responses, leading to:
- A reduction in the severity of illness
- Increased viral transmissibility
- A change in the effectiveness of vaccine and monoclonal antibody products
Though a genetically obsolete antibody may be unable to identify future SARS-COV-2 variant infections, they still signal the immune system in other ways discussed below.
Persisting virus after infection
Unfortunately, scientists have discovered that even after clinical recovery, elimination of detectable infectious virus, and the development of immunity, our body’s may still struggle to get rid of all the viral genetic material (viral RNA) inside infected cells. The difficulty of the body to remove all the viral RNA from cells may help explain why some people still experience symptoms of inflammation long after acute infection.
Immune dysregulation
Scientists have determined that antibodies to the SARS-Cov-2 spike protein have genetic sequences similar to dozens of tissue types in the human body. Because of this “molecular mimicry,” circulating COVID-19 antibodies can trigger immune responses to the person’s own tissue, causing a new autoimmune-like illness, with many patients forming new antibodies to their own body.
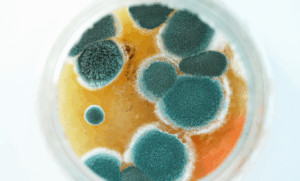
What’s more, numerous studies now indicate that inflammation from the COVID-19 spike protein causes a downregulation of the immune response to long-suppressed infections, allowing for reactivation of chronic viruses and biological toxins like Epstein-Barr Virus (EBV), Cytomegalovirus (CMV), Human Herpes Virus, Lyme infection, and chronic mold toxins.
Some groups of people who’ve had COVID-19 end up with similar symptoms to people with fibromyalgia, rheumatic conditions, and chronic fatigue, which are thought to be related to immune exhaustion from chronic viral or toxin inflammation.
Furthermore, there’s increasing data showing that some immune dysfunction is correlated with increased difficulty handling new viral and bacterial exposures (like the current RSV and influenza surges) or greater challenges with the routine removal of the normal cellular mutations that every person must deal with in order to prevent the “mutiny” of cancer.
Importantly, it’s been long established that viruses can induce cancer. Well-known examples include:
- Hepatitis C virus and heptocellular cancer
- HIV and lymphomas
- Human Papillomavirus (HPV) and cervical cancer
Gut microbiome imbalances
Accumulating evidence also shows significant alterations to the gut microbiome composition of patients with long-term complications from COVID-19. The microbiome is directly related to host immunity and is an important component of investigation and therapeutic attention.
Yes, it’s all rather complex (let’s take a deep breath.)

Even as you read this, medical science is learning more each week about this diagnosis. The entire ViveWell team wants to keep you up-to-date about emerging care that may offer hope to those of you suffering from this health challenge.
At this point, you’re probably wondering what can be done to help you feel better. We can’t wait to show you.
ViveWell — your partner in long-COVID care
At ViveWell, we use comprehensive protocols specialized in treating all the systems affected by COVID and other ailments. We care for you using the best information and interventions available, and our ultimate goal is to restore your body to its natural, optimally balanced state — returning you to health and well-being.
We deliver a combination of holistic health evaluation and individualized, data-informed treatment plans based on scientifically verified therapies. We care for you with precision medicine that acts at the cellular level to rejuvenate feelings of wellness and restore health.
At ViveWell, our cutting-edge treatments do more than restore hope. They help to actually restore the health that you’ve been missing for months or years. We know the frustration people experience when whatever they’ve been doing isn’t working. Now is the time to take the first step to regaining the life you long to live.
Are you ready to invest in getting your life back? We can help. The medical providers at ViveWell are ready and committed to helping you feel better.
Contact our team today with questions or to begin working toward a healthier, more rejuvenated you.
References
- Block, T, & Kuo, J. (2022) Rationale for Nicotinamide Adenine Dinucleotide (NAD+) Metabolome Disruption as a Pathogenic Mechanism of Post-Acute COVID-19 Syndrome. Clinical Pathology, 15. https://doi.org/10.1177/2632010X221106986
- Cabral-Marques, O., Halpert, G., Schimke, L. F., Ostrinski, Y., Vojdani, A., Baiocchi, G. C., Freire, P. P., Filgueiras, I. S., Zyskind, I., Lattin, M. T., Tran, F., Schreiber, S., Marques, A. H., Plaça, D. R., Fonseca, D. L., Humrich, J. Y., Müller, A., Giil, L. M., Graßhoff, H., … Shoenfeld, Y. (2022). Autoantibodies targeting gpcrs and Ras-related molecules associate with COVID-19 severity. Nature Communications, 13(1). https://doi.org/10.1038/s41467-022-28905-5
- Fajgenbaum, DC, & June, CH. (2020). Cytokine Storm. New England Journal of Medicine; 383: 2255-2273. DOI: 10.1056/NEJMra2026131 https://www.nejm.org/doi/full/10.1056/NEJMra2026131
- Groff, D, Sun, A, Ssentongo, AE, et al. (2021). Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2 Infection: A Systematic Review. JAMA network open, 4(10), e2128568. https://doi.org/10.1001/jamanetworkopen.2021.28568
- Halpert G, Shoenfeld Y. SARS-CoV-2, the autoimmune virus. Autoimmun Rev. 2020 Dec;19(12):102695. doi: 10.1016/j.autrev.2020.102695. Epub 2020 Oct 28. PMID: 33130000; PMCID: PMC7598743. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7598743/
- National Institutes for Health (NIH). (n.d.) Syndrome. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/syndrome
- Patterson, BK, Guevara-Coto, J, Yogendra, R, et al. (2021). Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning. Frontiers in Immunology. https://doi.org/10.3389/fimmu.2021.700782
- Perico L, Morigi M, Galbusera M, Pezzotta A, Gastoldi S, Imberti B, Perna A, Ruggenenti P, Donadelli R, Benigni A, Remuzzi G. SARS-CoV-2 Spike Protein 1 Activates Microvascular Endothelial Cells and Complement System Leading to Platelet Aggregation. Front Immunol. 2022 Mar 7;13:827146. doi: 10.3389/fimmu.2022.827146. PMID: 35320941; PMCID: PMC8936079.
- Buzhdygan TP, DeOre BJ, Baldwin-Leclair A, Bullock TA, McGary HM, Khan JA, Razmpour R, Hale JF, Galie PA, Potula R, Andrews AM, Ramirez SH. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood-brain barrier. Neurobiol Dis. 2020 Dec;146:105131.doi:10.1016/j.nbd.2020.105131. Epub 2020 Oct 11. PMID: 33053430; PMCID: PMC7547916.
- Vojdani, A., Vojdani, E., Melgar, A. L., & Redd, J. (2022). Reaction of SARS-COV-2 antibodies with other pathogens, vaccines, and food antigens. Frontiers in Immunology, 13. https://doi.org/10.3389/fimmu.2022.1003094
- Jacobs, J. J. L. (2021). Persistent SARS-2 infections contribute to long covid-19. Medical Hypotheses, 149, 110538. https://doi.org/10.1016/j.mehy.2021.110538
- Gold, J. E., Okyay, R. A., Licht, W. E., & Hurley, D. J. (2021). Investigation of long covid prevalence and its relationship to Epstein-Barr virus reactivation. Pathogens, 10(6), 763. https://doi.org/10.3390/pathogens10060763
- Simonnet, A., Engelmann, I., Moreau, A.-S., Garcia, B., Six, S., El Kalioubie, A., Robriquet, L., Hober, D., & Jourdain, M. (2021). High incidence of Epstein–Barr virus, cytomegalovirus, and human-herpes virus-6 reactivations in critically ill patients with covid-19. Infectious Diseases Now, 51(3), 296–299. https://doi.org/10.1016/j.idnow.2021.01.005
- Griffin, D. E. (2022). Why does viral RNA sometimes persist after recovery from acute infections? PLOS Biology, 20(6). https://doi.org/10.1371/journal.pbio.3001687
- Verma, D., Church, T. M., & Swaminathan, S. (2021). Epstein-Barr virus lytic replication induces ACE2 expression and enhances SARS-COV-2 pseudotyped virus entry in epithelial cells. Journal of Virology, 95(13). https://doi.org/10.1128/jvi.00192-21
- Wang, B., Zhang, L., Wang, Y., Dai, T., Qin, Z., Zhou, F., & Zhang, L. (2022). Alterations in microbiota of patients with covid-19: Potential mechanisms and therapeutic interventions. Signal Transduction and Targeted Therapy, 7(1). https://doi.org/10.1038/s41392-022-00986-0
- Liu, Q., Mak, J. W., Su, Q., Yeoh, Y. K., Lui, G. C.-Y., Ng, S. S., Zhang, F., Li, A. Y., Lu, W., Hui, D. S.-C., Chan, P. K. S., Chan, F. K., & Ng, S. C. (2022). Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut, 71(3), 544–552. https://doi.org/10.1136/gutjnl-2021-325989
- News Center (2021) Study links severe COVID-19 to increase in self-attacking antibodies, News Center. Available at: https://med.stanford.edu/news/all-news/2021/09/covid-19-autoantibodies.html (Accessed: December 5, 2022).
- Sidik, S.M. (2022) Heart disease after Covid: What the data say, Nature News. Nature Publishing Group. Available at: https://www.nature.com/articles/d41586-022-02074-3#:~:text=These%20clots%20can%20clog%20blood,people%20who%20had%20had%20influenza. (Accessed: December 5, 2022).
Share on:
Relevant blogs

Unlock the Potential of Hormone Optimization
In a world where medical science continues to make remarkable strides, one revolutionary therapy has emerged as a promising option
TruDOSE PRP Therapy at ViveWell Health: Level up with Precision Platelet-Rich Plasma Therapy
ViveWell Health has offered platelet-rich plasma therapy, commonly known as PRP, to those searching for a regenerative treatment that supports
Mold, Metals, and Metabolic Health
When people think about their health, they often focus on symptoms like fatigue, joint pain, brain fog, or stubborn weight

Integrative & Functional Nutrition Therapies: The Cornerstone of Optimizing and Sustaining Men’s Health
Men’s metabolic health, weight balance, gut integrity and sexual health and vitality, all hinge on one core principle: the strategic

Integrative regenerative optimized healing
Located in beautiful Colorado, our clinic offers holistic customized treatment programs to improve and restore your health. For more information or to schedule your consultation, please contact us today. We’re here to answer any of your questions.
Disclaimer: All statements and opinions provided are for educational and informational purposes, not for medical diagnosis. As with all medical treatments and procedures, results may vary on an individual basis. ViveWell follows all FDA guidelines related to the treatments provided. You’re encouraged to consult with your primary care provider before undergoing any treatment programs offered by ViveWell. Some of our therapies are not FDA-approved. During your personal consultation, the benefits and risks of any recommended therapies will be reviewed with you.
Prices are subject to change.